A New Jersey federal judge granted summary judgment to Bristol Myers-Squibb in a Plavix lawsuit which alleged that the blood thinner was responsible for plaintiff’s gastrointestinal bleeding. Interpreting California law, the District Court relied on learned intermediary doctrine (Case Chaiken v. Squibb, In Re: Plavix Mktg., Sales Practices & Products Liability Litigation).
The plaintiff argued that the injuries she had to endure resulted from the negligent design, manufacture, development, labeling and marketing of the anticoagulant medication Plavix (clopidogrel). According to her claim, the manufacturers failed to adequately warn her doctors about the potential dangers of this medication, causing her to suffer personal damage and injuries.
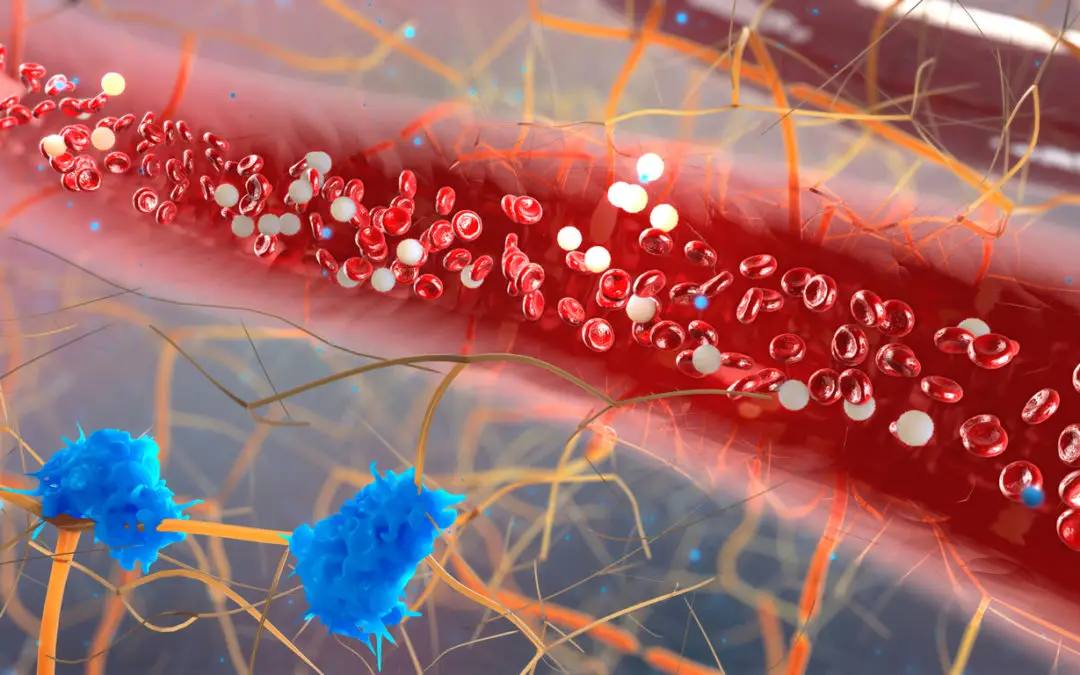
Plavix is an antiplatelet drug prescribed to high-risk patients who suffer from peripheral arterial disease, angina pectoris, or who have been implanted with a coronary artery stent to reduce the risk of blood clots, heart attacks and strokes. Several litigations have been filed so far by patients who allege that the drugmakers falsely advertised clopidogrel as a superior alternative to aspirin. Additional allegations of misrepresentation involved almost 1,000 plaintiffs so far, although, to date, some 5,000 total victims filed a claim across the country.
According to law, the plaintiff must provide the court with sufficient evidence showing that an undisclosed risk might have affected a physician’s decision to prescribe the medication. The victim focused on a declaration of her neurologist, who, after reviewing a clinical trial, warned her about a risk of recurrent bleeding ulcers associated with Plavix rather than with aspirin. The plaintiff argued that this specialist’s statement might have changed her physician’s decision to prescribe this anticoagulant medication.
However, the District Court rejected plaintiff’s assertion and barred her claims for design defect and failure to warn. In fact, her two physicians testified that she was intolerant to aspirin, so regardless of the bleeding risk, they would have prescribed clopidogrel anyway. The neurologist, on the other hand, was not the prescribing doctor during the period when the victim suffered her gastrointestinal bleeding. After she was discharged from the hospital, the only doctor responsible to prescribe any drug was thus her primary care physician.
Article by Dr. Claudio Butticè, Pharm.D.